Shannon Thyne’s little brother could barely walk when she met him.
At just 2 years old, his legs trembled beneath him — unsteady from an early life confined to a crib.
He showed other signs of a difficult infancy. He was accustomed to talking to himself, a habit born from loneliness, with a father behind bars and a mother battling addiction. He ate every meal as if it were his last, stuffing himself until his stomach revolted.
Thyne was just a fourth grader when her parents adopted her brother from the Los Angeles County foster care system. She understood, even then, that her brother had been shaped by something invisible yet deeply rooted.
It would take decades for science to catch up to what Thyne sensed: Childhood adversity imprints itself on the body. And it does not fade easily or quickly.
Thyne’s mother, a teacher at the time, built her son’s world from the ground up. She created structured routines to nurture a sense of consistency. She taught him how to eat in a regulated manner. She enrolled him in piano lessons to develop his fine motor skills. She enforced a disciplined bedtime routine to bring order to his restless nights.
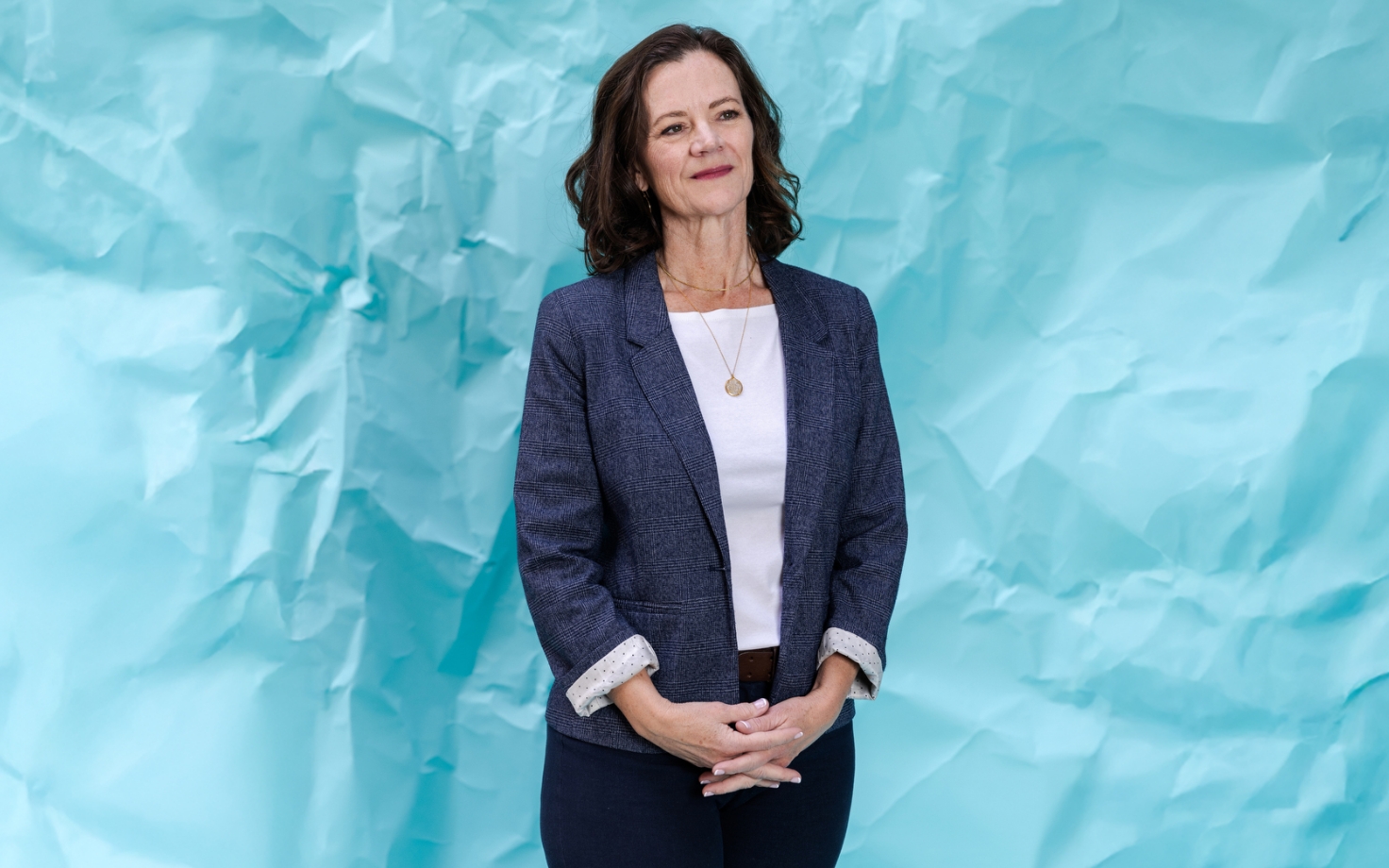
Years later, Thyne took that knowledge from her childhood home into the heart of medicine. Today, serving at the helm of trauma-informed pediatric care in Los Angeles, she spearheads efforts to reimagine the way healthcare providers identify and respond to childhood adversity.
At the core of that mission is UCAAN — the UCLA/UCSF ACEs Aware Family Resilience Network — a program that integrates a screening system known as “Adverse Childhood Experiences” or ACEs. Healthcare providers screen for ACEs to assess exposure to potentially traumatic events in a child’s life. ACEs are broadly categorized into three groups: abuse, neglect and household challenges. By identifying experiences early, doctors can work toward providing patients with adequate resources to mitigate long-term health risks associated with childhood adversity.
The ultimate goal? To make trauma and mental health as much a part of children’s medical records as their blood pressure and weight.
“When I went to my doctor, she had me do my diabetes screen, my cholesterol screen, my blood pressure screen, my mammogram,” Thyne said. “And hopefully — and she does — she checks in on my mental health and my social safety. She asks me if I’m in a safe relationship, if I have sexual safety, if I have all those things. And ACEs is one way to do that, and it’s a way that’s evidence-based.”
Trauma’s effect on bodies and minds
A native of Los Angeles, Thyne initially set out to study psychology at Yale University. But studying abroad in France in her junior year during the AIDS epidemic convinced her to switch her major to biology. She attended medical school at Brown University and completed her residency at the University of California, San Francisco. There, she turned her work toward the use of medicine to address trauma.
Now, she’s making evidence-based, trauma-informed care a pillar of pediatrics. She is the chief of pediatrics at Olive View-UCLA Medical Center, and the director of pediatrics for the L.A. County Department of Health Services.
Her approach starts with the observation that childhood trauma can rewire bodies as much as it can sculpt minds. The scars of early-life adversity often run deeper than memory — silently but profoundly altering the body, raising the risk of illness and stealing years before they’re lived.
“People have come to recognize that healthcare is more than shots and medication,” Thyne said. “Not only does stress or toxic stress … impact your psychosocial health, like make you more anxious or more likely to have substance use disorder, it [also] actually increases your chances of dying from heart disease, getting diabetes, having asthma flares.”
The ACEs screening process involves patients answering a questionnaire to generate an ACE score, which acts as a medical roadmap. It is indicative of a child’s exposure to childhood adversity, with a higher score signaling greater health risks. Pediatricians then use scores to connect families with the right support, helping break cycles of trauma before they take root.
UCAAN operates on the notion that primary care providers are well-positioned to intervene. Pediatricians, after all, see children from infancy through adolescence, often forming some of the most stable relationships in a child’s life. If they can identify children with high ACEs early, they can connect families to services that buffer the effects of toxic stress — before they become chronic.
Nadine Burke Harris, in partnership with the California Department of Health Care Services (DHCS), pioneered an initiative in 2021 — the first of its kind — to screen for childhood trauma and treat toxic stress at its root.
Medi-Cal providers trained under the ACEs Aware initiative receive a $29 reimbursement per screening — funded through Medi-Cal, which is supported by both state and federal contributions. Through UCAAN, California has screened more than 4 million patients for ACEs, providing critical data on the prevalence of childhood adversity.
But while pediatrics lead the way in trauma-informed care, adult medicine is catching up. UCSF’s Dr. Edward Machtinger — co-principal investigator of UCAAN alongside Thyne — said internists play an indispensable role in rupturing the generational cycle of trauma by healing caregivers.
“Internists have the most powerful role in the healthcare system to reduce childhood trauma by helping adult parents and caregivers heal from the impacts of their own trauma, like substance use and mental illness,” Machtinger said, “and, in that way, interrupt generational cycles of trauma.”
As the program elicits more and more information and is embraced more widely by the medical community, supporters have set their sights on social transformation.
“We continue making progress toward our goal of cutting ACEs and toxic stress by half in a generation,” Harris, a former California surgeon general, said after enacting Senate Bill 428, which expanded coverage for ACEs screening.
Toward an integrated response
Asked which UCANN program has made the biggest impact on her, Thyne did not hesitate: SHARK, she said.
SHARK — Strong, Healthy and Resilient Kids — redefines care for children facing trauma and complex health challenges. By integrating pediatricians, psychiatrists, physical therapists and social workers, the grassroots program attempts to build individualized support systems, whether through ADHD management, anxiety-reducing meditation programs or in-home visits that connect families with essential resources.
Employed at Rancho Los Amigos National Rehabilitation Center in Downey, SHARK relies on the full range of access points and services. Patients can connect using virtual visits, but also can receive hands-on support through after-school programs and special education resources. SHARK starts by asking doctors to think differently about a child’s issues.
“One of the best ways I have found is to move from asking yourself what’s wrong with somebody,” Machtinger said, “to asking what happened to them.”
From there, the goal is to secure the right help. “Say I have a kid who’s got pretty bad anxiety, and maybe a little ADHD. I can refer them to SHARK. We’ll see them for a virtual visit and say, ‘Oh, wow, you’ve got a lot going on. Let me send a community health worker to your house, and we’ll help you get set up with food boxes,’” Thyne said. “And, ‘Oh, man, your ADHD is really acting up, let’s help you find a psychiatrist that can give you your medications.’ And ‘Oh, your brother has down syndrome?’ Okay, well, let’s refer him to TASK (Treatment Advocates for Special Kids) so that we can make sure he gets all of his school accommodations.”
One particularly successful pilot project involved an online meditation program for children with anxiety and depression. After 10 virtual sessions, children saw measurable improvements in their GAD-7 — an anxiety score — and their PHQ-9, a depression score.
“Someone gets screened for ACEs, someone ends up in a specialized program because after their screen for ACEs, someone said they had anxiety and depression, and that specialized program SHARK said, ‘Maybe you’d benefit from this program that we found in the community.’ They enroll them in that, then — back to the academics — they investigate that, and the data says they got better,” Thyne said.
Fires that tore across Southern California in January seeped into every corner of children’s lives. Ash settled on textbooks, smoke curled into classrooms, and evacuation orders turned homework and recess into an afterthought.
Some children watched from car windows as flames consumed the only world they knew — their routines and sense of safety dissolving in smoke — and others lost the simple certainty of a safe place to sleep. The scent of burning brush will cling to their clothes long after flames died down.
That is trauma at its most basic.
“It’s a great example of another ACE,” Thyne said. “Kids do really well with routines and normalcy, and it’s going to be a long time until they get to routines and normalcy. Kids are really influenced by the mental health of their caregivers, so for caregivers — even though it’s not an ACE for an adult because ACEs are for kids — it is a lot when your parents experience something like this.
“We don’t want to protect kids from the truth, but we also need to help them figure out how to feel safe.”
Thyne emphasized that care isn’t a one-size-fits-all. A UCLA student grappling with fears of air quality or an upcoming exam demands different support than a child in a small town who’s been displaced from home and school.
UCAAN’s mission in all of this is to reframe how we view trauma and offer support tailored to individuals based on their own experiences.
“As you can tell, I love my job. At the end of the day, one of my favorite things is just to sit on the floor in a patient room, watching a kid learn how to walk,” Thyne said. “Those things are still super fun. But when you also say, ‘Oh, I helped you get your wheelchair ramp for your mom, who has multiple sclerosis, and we helped get you better housing, and that’s going to make everyone’s mental health better.’
“Those things,” she added, “are a huge part of it, too.”